Smash a melon, NOT my Boob!
Is DCIS Cancer?
DCIS or Ductal Carcinoma in Situ, Stage 0 breast cancer, or pre-cancer is the most common “breast cancer” diagnosis for women. Found on a routine mammogram as tiny clusters of calcifications (microcalcifications)—small white specks that may suggest abnormal cell growth, it is diagnosed via stereotactic breast biopsy as low, intermediate and high grade as determined by cellular size, shape, growth pattern. A The National Breast Cancer Coalition defines DCIS as NOT CANCER. However, nearly all women diagnosed with DCIS receive treatment, most commonly surgery—either lumpectomy or mastectomy along with radiation and hormonal therapy. In fact, up to one-third undergo mastectomy and the rate for contralateral prophylactic mastectomy (where a healthy breast is also removed) has been steadily increasing.
Stage 0 Breast Cancer
Should DCIS be called cancer?
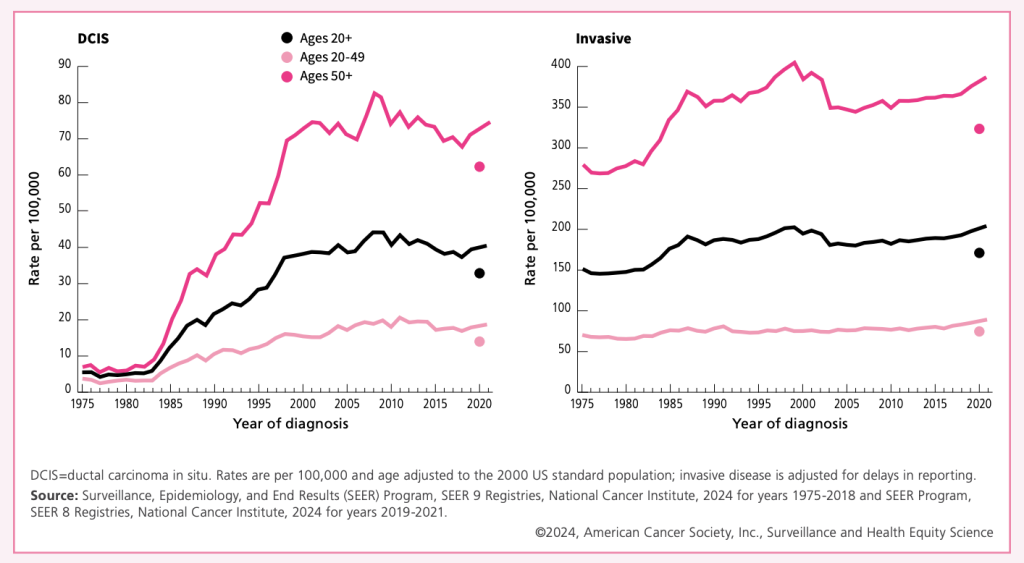
DCIS is non-invasive and may not warrant the label “carcinoma.” Reframing the language and approach could spare women unnecessary treatment and anxiety, focusing instead on careful monitoring and informed decision-making. Redefining DCIS could prevent overtreatment, reduce fear, and give women more balanced choices. There is an ongoing debate among researchers and clinicians about whether ductal carcinoma in situ (DCIS) should even be called “carcinoma.” By definition, carcinoma implies invasive cancer that can spread and threaten life, yet DCIS cells remain confined within the milk ducts and often never progress. Many experts argue that labeling it “carcinoma” creates unnecessary fear and leads to overtreatment. Decades of aggressive DCIS treatment have not lowered invasive cancer rates or breast cancer mortality, proving that DCIS is overtreated without impacting survival. In fact, among women younger than 50 years, there has been a 290% increase in DCIS since 1983 and incidence continues to rise. Are we getting sicker or is DCIS overtreated and overdiagnosed?
“DCIS is not cancer. It is a risk factor for cancer.” — Dr. Laura Esserman,When Cancer is NOT Cancer, The California Sunday Magazine, 2014
Somehow DCIS ended up in the cancer camp rather than the risk-factor camp, and all my work is to push it back.” — Dr. Shelley Hwang, The Danger of DCIS, The Breast “Cancer” That’s Often Not, Elle Magazine, 2015
“DCIS is a marker for breast cancer risk; it itself is not cancer. Removing the speedometer does not change the speed of the car, so removing DCIS, irradiating it, or giving it pills will not change the risk of dying.” – Dr. Jennifer Marti, Ductal Carcinoma In Situ: The Weight of the Word “Cancer,” AACR, October 12, 2022
“DCIS — “In and of Itself is not a ‘cancer’ lesion.” – Hal Burstein, M.D., Ph.D., clip from Peter Attia, MD Podcast 278 ‒ Breast cancer: how to catch, treat, and survive breast cancer, Nov. 6, 2023
In 2010, the American Cancer Society and NCI convened a workshop to consider changing the name and improving risk communication. Is DCIS Cancer? Rethinking the “Carcinoma” in Stage Zero Breast Cancer references the following resources on the contreversy behind the Ductal Carcinoma in Situ label:
- A Major Shift in Breast Cancer Understanding (Time, 2015)
- What’s in a name—is DCIS cancer? From Ductal Carcinoma in Situ: Current Concepts in Biology, Imaging, and Treatment (J Breast Imaging, 2019)
- Renaming Ductal Carcinoma in Situ: Would Removing “Carcinoma” Reduce Overtreatment? (JNCCN, 2014)
- How different terminology for ductal carcinoma in situ (DCIS) impacts women’s concern and management preferences: A qualitative study (Science Direct, 2015)
- The sea of uncertainty surrounding ductal carcinoma in situ–the price of screening mammography (J Natl Cancer Inst, 2008)
- Ductal Carcinoma In Situ , Complexities and Challenges (JNCI, 2004)
- Ductal carcinoma in situ: to treat or not to treat, that is the question (BJC, 2019)
- Treatment of low-risk ductal carcinoma in situ: is nothing better than something? (The Lancet Oncology, 2016)
- What is DCIS, and Why Does It Matter? (NBCC Website)
- When Cancer Isn’t Cancer (N1X10 Pickler, 2025)
- Challenges in DCIS Risk Communication and Decision-Making: Report from an American Cancer Society and National Cancer Institute Workshop (CA Cancer J Clin, 2014)
COMET Study
Latest DCIS research
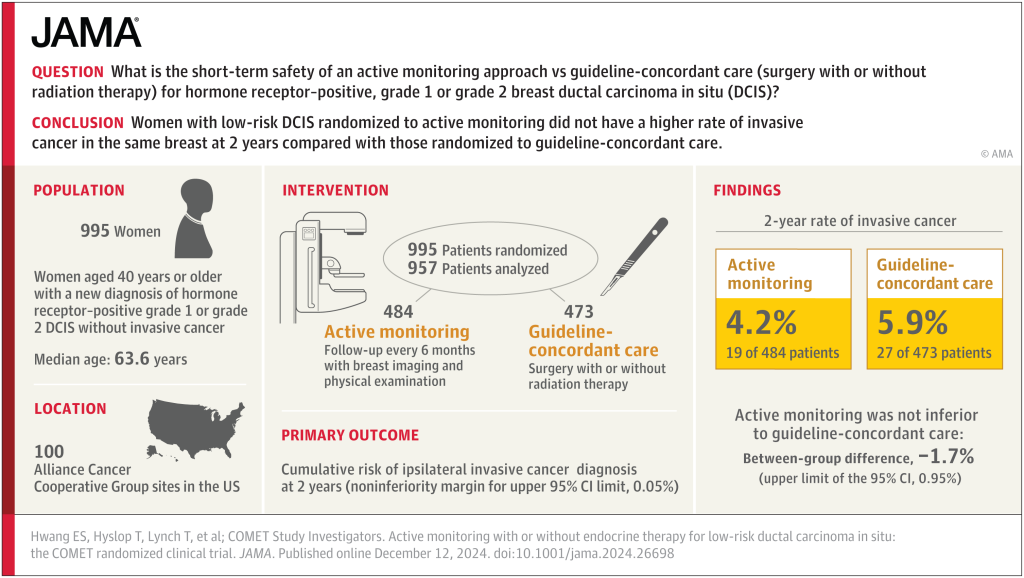
The COMET study provides compelling evidence that active monitoring can be a safe and effective alternative to surgery and radiation for certain patients with low-risk DCIS. The study enrolled 995 women aged 40 and older with low-risk, hormone receptor-positive, HER2-negative DCIS, randomly assigning them to either active monitoring or guideline-concordant surgical care. At the two-year follow-up, results revealed that the rate of invasive breast cancer in the same breast was lower in the active monitoring group (4.2%) than in the surgery group (5.9%), suggesting that careful monitoring may actually reduce the risk of progression compared with immediate surgery. Beyond cancer outcomes, patients under active monitoring reported similar or better physical, emotional, and psychological well-being than those who underwent surgery, highlighting that avoiding invasive treatment can significantly improve quality of life. Additionally, active monitoring reduces exposure to the potential harms of surgery and radiation, including pain, complications, and overtreatment, while achieving outcomes that are at least equivalent—and in some cases superior—to surgery.
The COMET study is part of a broader international effort to explore less invasive options for managing low-risk DCIS:
LORIS (UK): A trial assessing active surveillance versus surgery for low-risk DCIS.
LORD (Europe): A European study examining the same question.
JAPAN DCIS Trial: Investigating active monitoring in Japanese patients with low-risk DCIS.
These studies collectively contribute to a growing body of evidence suggesting that active monitoring may be a viable option for certain patients with low-risk DCIS.
DCIS Overtreatment
DCIS Active Surveillance
Since the release of the COMET trial results, leading medical journals, cancer centers, and professional associations have begun to question the routine use of surgery for ductal carcinoma in situ (DCIS). A growing body of evidence now shows that active monitoring can be just as safe—and in some cases better—than surgery, while also reducing unnecessary treatment and preserving quality of life. The following articles and expert commentaries highlight this shift and provide resources for patients and clinicians considering active surveillance.
JAMA Oncology – Active Monitoring With or Without Endocrine Therapy for Low-Risk DCIS Official COMET trial publication reporting equivalent or better outcomes with active monitoring. 👉 Read on JAMA
AAFP (American Academy of Family Physicians) – POEMs: Active Monitoring vs Surgery for DCIS Bottom line: active monitoring is a safe, non-inferior alternative to surgery. 👉 Read on AAFP
American College of Surgeons (ACS Brief) – Is It Time to Abandon Surgery for Low-Risk DCIS? Commentary following COMET asking if monitoring should replace surgery for many patients. 👉 Read on ACS
ObG Project – Can Women With Low-Risk DCIS Undergo Active Monitoring Instead of Surgery? Clear summary showing monitoring is noninferior to surgery with fewer risks. 👉 Read on ObG Project
Cancer Network – Active Monitoring May Be Safe vs Surgery in Certain Low-Risk DCIS Populations Expert commentary at Miami Breast Cancer Conference, supporting surveillance for select patients. 👉 Read on Cancer Network
Dana-Farber Cancer Institute – Quality of Life Maintained With Active Monitoring for DCIS No significant differences in quality of life, anxiety, or depression between monitoring and surgery. 👉 Read on Dana-Farber
AACR News Release – Quality of Life Similar Among Patients Choosing Monitoring or Surgery COMET confirms monitoring as a reasonable option without negative emotional effects. 👉 Read on AACR
Reuters – Surgery May Be Unnecessary for Common Precancerous Breast Condition Coverage of COMET results: progression rates similar or better with monitoring vs surgery. 👉 Read on Reuters
AP News – Active Monitoring Safe Alternative for DCIS Mainstream report on SABCS 2024 data showing surveillance is a valid treatment option. 👉 Read on AP
Our Stories

Smash a melon, mot my boob!
Disclaimer
The information provided on Smash a Melon, NOT My Boob! is for educational and awareness purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. We are not medical professionals.
Always seek the advice of a qualified healthcare provider regarding any medical condition, screening decision, or treatment option.
Connect with us today and join our challenge!
Subscribe
Join the conversation
Help us smash the silence.